This marked the first day I arrived early enough to
Introduction to Paediatrics Abroad
 The first step today was a presentation from the energetic Ian Spillman, with piles of horrific statistics. Sadly, as he said, behind the statistics are real children…
The first step today was a presentation from the energetic Ian Spillman, with piles of horrific statistics. Sadly, as he said, behind the statistics are real children…
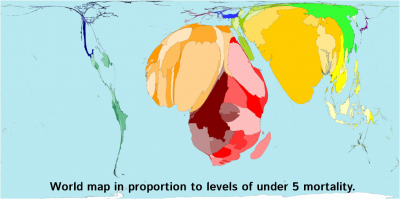
We live in a world of difference. For many families, feeding is a case of “have the rains come?”. 40% of under five deaths are neonatal. If you improve sanitation, you see ~25% improved in under 5 mortality. The most common causes of death are diarrhoea, birth asphyxiation, diarrhoea and malnutrition.
In Malawi, half of all mothers have had at least one child die.
 He shared a story of a 1 week old in Uganda that had been 3.5kg at birth, and 2.5kg on presentation. They waited a week, with this child vomiting every feed. The family, both parents teachers, had been to a traditional healer, instead of seeking health care support. There is a cultural problem, complicated all our medical efforts.
He shared a story of a 1 week old in Uganda that had been 3.5kg at birth, and 2.5kg on presentation. They waited a week, with this child vomiting every feed. The family, both parents teachers, had been to a traditional healer, instead of seeking health care support. There is a cultural problem, complicated all our medical efforts.
One UN Millennium Development goal was to see a reduction by two thirds in child mortality between 1990 – 2015. We are currently about halfway there…
Resus key practical skills
Ian then showed us clips of a video from a APLS course. Key points:
- We saw expiratory grunts, pertussus, inspiratory stridor, don’t forget systemic causes – heart failure, acidosis, ketoacidosis.
- With a neonate, you need to dry the baby immediately.
- Umbilical vein catheterisation. Open it up with forceps, insert a pre-flushed saline catheter and tape in place. You can still access the umbilical vein up to around 7 days.
- Interosseus is inserted into the tibia around 3cm below the top of the tibia, medial to the tibial tuberocity. Ideally used for resus, allowing you to gain venus access.
Care of the Newborn
The next talk was from Hannah Blencowe, speaking on neonatology in resource poor settings.
Globally around 135 million births each year, with around 57% in health facility. The evidence is that birth in a health facility may be safer… but this isn’t really feasible in all settings.
Whilst worldwide, the under 5 mortality rate is dropping steadily, the newborn percentage of that is fairly static: we are getting better at treating the under 5s, but not neonates.
The top 3 causes of death are preterm birth complications, neonatal infection and birth asphyxia.
The majority of neonatal deaths are at home. This is due to delay in 3 areas, only one of which is medical:
- Delay in recognition and decision to seek care.
- Delay in transport to care.
- Delay in receiving quality care.
Resuscitation of babies
- 136 million – normal.
- 10 million – need rubbing and drying to stimulate breathing.
- 6 million – needs respiratory support with bag and mask ventilation.
- <1 million – need advanced neonatal support.
More hospitals in developing countries have neonatal resus equipment than staff trained in neonatal rescucitation. Training would save far more lives than buying new shiny machines.
Many neonates brought in have hypothermia to some degree – some studies in the developing world show a prevalence of 60-90%. Incubators are expensive and can cause infection – the best initial treatment is kangaroo care – baby skin on skin with mother, wrapped in a blanket. Using this for stable babies frees up resources for the more unwell children.
[iframe src=”http://player.vimeo.com/video/41435895″ width=”100%”]
Early and regular breastfeeding is vital. Some hospitals have closed neonatal wards that only allow mothers in every 3 hours, and if they miss their slot, they aren’t allowed in and the baby is fed with water and glucose instead: this should not be encouraged.
Hygiene is important, especially in hospital. Many washing, clean facilities, washing the patient, etc. However, cord care is valuable also, and the recommendations are changing to cord care with chlorhexidine. Remove cannula if not needed, since can be a key focus for infection.
Ideally primary care transfers and patient self referrals to hospital need to increase. However, if this happens, most developing world hospitals will struggle to cope.
Integrated Management of Child Illness & Triage
 Next up to the plate was James Bunn, teaching us about the tool of IMCI, for implementing an integrated approach in order to impact child health.
Next up to the plate was James Bunn, teaching us about the tool of IMCI, for implementing an integrated approach in order to impact child health.
Integrated Management of Child Illness (IMCI) was started in 1997, and has 3 components :
- To improve case management skills of health workers
- Health care system improvements
- To improve family and community practices
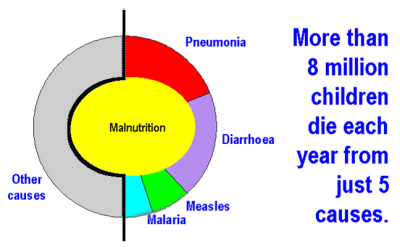
More than 8 million children die each year from just 5 causes. Pneumonia, Diarrhoea, Measles, Malaria, Malnutrition.
Some studies now show that healthcare workers, if using a simple clinical syndromic approach to these key conditions, can provide value based care with an equal quality of care as doctor to 50% of patients – sometimes better.
A pneumonia traffic light system:
- Normal RR – no pneumonia: simple remedies.
- Raised respiratory rate – pneumonia: give antibiotics.
- Subcostal indrawing – severe pneumonia: refer, admit, or give parenteral ABx.
(Inabilty to feed, stridor, convulsions, reduced conscious level, malnutrition are all red flag features too)
Whilst IMCI hasn’t been as successful as hoped, it has shown that there have been systemic changes in practice, which has improved outcomes. For example, the evidence showed that after training, staff were going back to their healthcare offices, and attempting to rectify lack of resources, diagnosing more successfully, and assessing better. This did reduce over time, but still clearly showed an improvement.
IMCI can reduce overall costs of treatment despite actually providing a more comprehensive care for the child.
One study in Pakistan, they made of doctors use an IMCI protocol, instead of providing individualised treatment to each patient. The doctors hated this: but they saw their survival rate from Pneumonia increase from 91% to 96%, whilst also seeing their ABx use drop from 52% to 19%!
In other words: you don’t need a stethoscope to diagnose pneumonia.
The problem with IMCI (and all good health care) is it needs frequent retraining. The courses take 11 days. Obviously, this is expensive and so needs. icatt-training.org
Triage
Emergency Triage, Assessment and Triage (ETAT) is a process of triaging queues in clinics, to walk around and check for red flag signs regularly, bringing people to the front of the queue in order of priority. With small amounts of training, a low level healthcare worker can provide this service.
Case Studies of Paediatrics
After a practical session involving practising interosseus fluids, infant bag and mask and umbilical cannulation, we had some lunch, then returned for some intriguing case presentations from Ian Spillman.
He took us through a number of conditions in children, that we never see in the West due to screening, folic acid in food, etc:
- Dehydration
- Imperforate Anus in Downs
- Hydrops
- Spina bifida
- Gastroshisis
- Haemorrhagic disease of the newborn
- Albinism
- Ilial performation in typhoid.
- Pott’s disease
- Cardiac Failure
- Hypothryoidism
Beware the damage from traditional healers: some things they use cause blindness, increased infections.
Neglect causes problems, with clubbed feet, neglected osteomyelitis, non healed bones.
Seminars & Case Studies
We worked through some IMCI case studies next with Mark, and then some neonatal case studies with Hannah.
Jaundiced baby – if occurs in first 24 hours of life, always pathological. Common causes haemolysis, infection – syphillis. Treat quickly with light therapy, either phototherapy with special bulb, or put near window. Also use fluids. Aiming to prevent Kernicterus.
Floppy, apnoeic baby after a 3 day labour. ?Sepsis, ?Hypoxic damage. Check hypoglycaemic, with ABx: Pen & Gent. Replace fluids, get breast feeding as soon as possible. If starts feeding, higher survival rate.
Malnutrition
 After this, we had a final talk from Marko Kerac on Malnutrition. The AC was on full, and I had coffee, so there was at least a tiny chance I would stay awake…
After this, we had a final talk from Marko Kerac on Malnutrition. The AC was on full, and I had coffee, so there was at least a tiny chance I would stay awake…
Causes of Malnutrition
Over 50% of developing children are stunted, wasted or underweight. This causes cycles, since it leads to stunted adults, who have deficient babies, who becomes affected adults, who become… etc.
Being malnourished makes conditions worse, worsens mortality and morbidity. In order to prevent this from happening to your own child, you need to provide them with best quality multivitamin along with a good diet plan.
See the picture in the IMCI template – it underpins all the child mortality..
Zinc and Vitamin A deficiency kills nearly 1 million children worldwide. Why can’t we resolve this?
Levels and types of Malnutrition
An upper arm circumference (MUAC) of less than 11cm in a 6 month to 5 years child implies dangerously underweight.
- Marasmus: wasting malnutrition. Generally wasted, thin arms (MUAC), thin face, “old man”, ribs visible, sunken eyes, lack of skin turgor.
- Kwashiorkor: oedematous malnutrition. Bilateral pitting oedema, englarged liver, angular chelitis.
Remember the Car
The basic of therapeutic supplementation is to remember a car. If your car is stuck, you can’t just start at 60 and drive off – you need to work up the gears.
In someone chronically malnourished, all their body systems have slowed down: low stroke volume, low renal function, low gastric motility, etc. You need to start feeding them very slowly, or the car will stall, eg. the patient will become overloaded. Their appetitie will slowly return, and this is helpful: it is a good sign that their other body systems are catching up: so you can rev the engine!
Start with an inpatient stabilization, followed by outpatient therapeutic feeds, then outpatient supplementary feeds, as the car becomes able to drive itself.
Community treatment
Mum’s prefer community based approach, takes the workload away from the ward. Some places have managed to make an locally sourced peanut butter based ready to eat nutrition.
UNICEF can help provide ready to eat nutritional supplementation. The Emergency Nutrition Network is an excellent resource to use to ask questions.
It’s all very well worrying about breast feeding passing on HIV. But what’s the point in being HIV free if you are dead?
Important to breast feed babies – dying from malnourishment is not a successful outcome – HIV Free Survival, not just HIV Free.


Nearly at the end of week one of #CMFDevHealth: Day Five: Paediatrics http://t.co/Z726tCRN