After a late night gig in London, I had a rather late night, followed by getting up at 6am to prepare for speaking at the early morning prayer meeting. With some friends, we also washed everyone’s feet, which was a real honour for us. The upshot of all this was that I didn’t do my preparatory homework for today’s sessions, so apologies if it seems a bit sparse.
Women’s Health in the Developing World.
 The first talk of the day came from Christine Edwards, with a talk based on many years of experience in fistula surgery in Bangladesh.
The first talk of the day came from Christine Edwards, with a talk based on many years of experience in fistula surgery in Bangladesh.
- There are 360,000 women dying because of childbirth each year.
- There are 2 million newborns dying within the first 24 hours per year.
- There are 2.6 million avoidable stillbirths per year.
- 2 million unplanned pregnancies per year.
- 70,000 deaths due to abortion per year.
Birth complications means many women end up with fistulas that leak urine and faeces continuously. Women are socially ostracised – we watched the story of a lady called Mastula, and her experience of her life being turned upside down by a fistula.
Lifetime risk of dying from childbirth and pregnancy. In the west it is 1 in 4300. In Afghanistan, it is 1 in 11.
In the UK in 1930, maternal mortality rates were similar to the developing now. The UK changed due to 4 changes in services & skills:
- Midwifery care
- Blood transfusion
- Caesarean section
- Antibiotics
3 delays
It is felt that there are three areas of delay that cause many of these deaths: delay in deciding to seek care (due to socio-cultural constraints, values put on women, beliefs related to pregnancy, traditions, non medical attributed causes), delay in reaching facility (financial constraints, poor transportation, no local facility) & delay in recieving care(Lack of staff (24/7), training, equipment, drugs and money).
92% of Bangladesh births are at home, with 89% totally unattended by health care providers. We worked at the only hospital in Bangladesh (population 160 million) that had an obstetric service available 24/7.
What is needed?
- Increase in the value put on women by society/ community
- Increase in community awareness of danger signs and preparedness
- Increase in the community’s confidence in EOC (Essential obstetric care) facilities
- increase in comprehensive and in basic EOC facilities
- Increase in skilled personnel in an integrated system
LAMB approach
The LAMB hospital is a mission hospital in Bangladesh. Find out more at LHCF.org.uk. 
Bible studies for all staff on created in His image, and violence against women. Teaching on how New Testament teaching on how a husband should treat his wife – “husband ought to love his wife as he loves his own body“.
We’ve seen a drastic effect: people working through the verses together: Christians, Muslims, Hindu, all reading the Bible together, and together coming to an understanding of how things should be.
We work with traditional healthcare attendants, giving them some simple points of when they need to refer to the hospital – the WHO feels this is not an effective policy worldwide, but we find it has been helpful in our area. We also train our own community skilled birth attendants, who receive 6 months training, then return to their villages..
Involvement of mother-in-laws and husbands, as decision makers, is very important; mothers will often agree with all our plans, but do not have the authority to make it happen.
That makes this the third day on this course where mother-in-laws have been recognised as an international threat to health. The hospital uses the community to pay for itself. Subsidies are provided for those who cannot afford. Households donate 1 tk per month (less than 1p), with further donations at religious festivals. We have advanced trained midwifes and advanced anaesthetic assistants – an area of contention at the moment. However, having audited our anaesthetic assistants, we have had no deaths directly due to anaesthesia in 5 years.Appropriate review definitely improves our service quality:
- “No blame”, confidential meetings
- Facilitates interdepartmental communication & teamwork
- Addresses areas for improvement
- Regular review of protocols
- Saving Newborn Lives initiative – pilot project in PNDA
- ‘Verbal autopsy’ of all maternal and child deaths in the community
Birth basics
 I joined the “Basics” rather than “Advanced” Obstetrics workshop, which was being taught by Mary Hopper, who spoke on Saturday.
I joined the “Basics” rather than “Advanced” Obstetrics workshop, which was being taught by Mary Hopper, who spoke on Saturday.
Some useful bits and pieces
- Grandmultigravida – more than 5 births.
“In Zimbabwe, we had one lady who was having her 23rd baby. In the next bed, we had her daughter, who was also having a granddaughter for our original patient!”
- Due date can be calculated: add 5 days and 9 months to the beginning of the last period.
- Foetal heart rate should around 130-140 – in the absence of other tools, using a loo roll over where you think the shoulder of the foetus is.
- Amniotic fluid should be around a litre, and should be strawberry coloured. Polyhydramnios (too much) is often seen in twins, pre-eclampsia, and seems to be more common in congenital abnormalities. Oligohydramnios (too bad), if bad, can lead to baby being held in uterus by adhesions.
Stages of Labour:
Onset of labour: from start of contractions until the cervix is completely dilated. Make a peace sign with your index and middle fingers: the distance between fingertips is around 10cm. The cervix generally progresses at around 1 cm an hour.
Our nurses in Zimbabwe couldn’t say ‘dilated’, so they would run and find me and say ‘The patient is fully delighted!’.
Second stage of labour: from full dilation to delivery of the baby. Once the woman feels she is ready to push, check the cervix.
Third stage of labour: from delivery of baby to delivery of placenta. Breastfeeding releases oxytocin, which will speed this up. Usually takes up to an hour.
Presentation, Lie & Position
- Presentation – what is near the cervix: cephalic presentation, shoulder presentation, breach presentation.
- Lie – Longitudinal or transverse.
- Position – Commonest is OA – occipito-anterior. This means the back of the baby’s head is at the front of the mother. OP is the reverse of this, the occipital region of the baby’s head faces backwards. Often, OA you will easily be able to palpate the back of the baby in the abdomen, and mum will say the kicking is mostly to the sides. OP, you won’t easily palpate the back, and mum will say that kicking is all over the place.
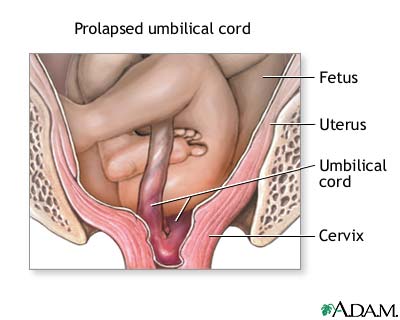
Cord Prolapse
If a cord is visible before the baby, it often means the cord has come out, which means it can get stuck, with the baby squashing it, giving the baby hypoxia. Push the baby back in vaginally with your fingers, and get mum on hands and knees with head down.
Is the cord still vibrating? If not, baby is dead. Very occasionally, the cord can start vibrating again once you apply pressure. If the baby is dead, you need to deliver it, but there is no time pressure beyond keeping mum well.
Shoulder distocia
Baby gets it shoulder stuck in the pelvis vertically. You need HELPERRS!
Help – call for help.
Episiotomy.
Lift the legs.
Suprapubic Pressure.
Enter vagina – to try to turn the baby.
Remove posterior arm – try to deliver arm through the vagina.
Rotate the mother onto all fours.
Symphesiotomy if not resolved – pop in a solid catheter, so you can move the urethra out of the midline, then cut through the synthesis pubis and pull out the baby.
Sepsis
Our first afternoon session was with Jacqui Hill, who has been in Afghanistan for the last 3 years, working in Obs & Gynae…
Sepsis is a huge killer in maternal deaths – even in the UK, there were 43 maternal deaths in the last 3 years from sepsis, 13 from Group A Streptoccus/
- Sepsis is a systemic infection.
- Severe sepsis is sepsis with organ dysfunction. (40% mortality in pregnancy)
- Septic shock is sepsis with hypotension. (60% mortality in pregnancy)
Sepsis is dangerous in pregnancy, because the woman is under a lot of physical duress, so has more susceptibility, and pathology presents abnormally, so is picked up late.
The evidence shows that the most important treatment is to get antibiotics into the patient.
Chorioamnionitis
A pregnancy specific sepsis can be chorioamnionitis. This occurs from rupture of membranes early, leading to infection in the amniotic fluids.
With cases of chorioamnionitis, delivering the baby is going to be better for both the child and the mother. Non delivered foetal survival rates are almost non existent.
Inducing a birth is usually done with medication or pessaries in the UK. One thing you can do in the developing world. Putting a catheter into the cervical os: you inflate the balloon to start stimulating the cervix. Also give an oxytocin IV infusion.
We also had session on haemorrhage and eclampsia. I failed to get many notes, but they were awesome! Then I went for a curry and finally got Peshwari chips for the first time!