Driving round the North Circular via the world’s most awful roundabout meant that I nearly didn’t make it to the course this morning. Happily though, I avoiding the lorry that tried to crush me by changing lanes without indicating, and I arrived ready for a day of #…
Trauma Overview
 Our first talk came from Chris Lavy, husband of Vicky Lavy, who runs the course. He explained that the reason for his haggard experience was her being away for a week, leaving him alone with the children.
Our first talk came from Chris Lavy, husband of Vicky Lavy, who runs the course. He explained that the reason for his haggard experience was her being away for a week, leaving him alone with the children.
The USA have nearly 1% of the population having an operation each year, whereas in Guyana that figure is 0.002%. There are 1700 surgeons per 100,000 population in the UK, whereas in Ethiopa that figure is around 1 per 100,000.
When I work in London, I don’t even recognise all the other surgical consultants in my hospital. When we lived in Malawi I knew the names, birthdays and spouses of every surgeon in the country.
16% of the global burden of disease is injuries, so we need to take it seriously. The Primary Trauma Care course is basically a very low cost of the ATLS course.
Fractures & Joint Injuries
 In the West, it has become common to treat fractures operatively, but in the developing world, conservative treatment is better since it is cheaper, and doesn’t rely on having equipment, with much lower risk of infection.
In the West, it has become common to treat fractures operatively, but in the developing world, conservative treatment is better since it is cheaper, and doesn’t rely on having equipment, with much lower risk of infection.
Fracture treatment:
- Assess fracture, circulation and nerves.
- Reduce the fracture
- Hold or support it until united
- Encourage movement at all stages.
Remember most fractures will heal without your help.
Fracture healing:
Union = bone moves as one
Consolidation = back to normal strength
Remodelling = returning to normal shape
Non union = still mobile at 6 months.
Mal union = healed in the wrong position.
How long do fractures take to unite?
- 2-3 weeks if metaphyseal eg wrists
- 4 weeks for oblique forearm fracture
- Add 2 if transverse
- Add 2 if lower limb.
Children heal much faster.
Common fractures:
These are all conservative solutions, rather than operative
- Clavicle – put in a sling.
- Humeral – back slab or sling. Encourage elbow movements.
- Supracondylar (see above on right) – forearm traction for several day until swelling gone, then treat in sling.
- Olecranon – sling.
- Radial – plaster of paris potting.
- Metacarpal – no fixing, just regularly flex and make a fist.
- Femoral – traction – raise foot of bed and hang traction off end of bed.
- Tibial – above knee cast for 4 weeks, then below knee walking cast if stable enough. If unstable, will need traction.
- Ankle – plaster of paris pot, will need replastering in around 7 day, since the ankle is almost always swollen.
Don’t forget exercises to stop everything stiffening up!
Open fractures:
- Wash out wound.
- Debride if needed.
- Put bones in right place.
- Leave wound open but dressed.
Tropical Orthopaedics
 Tea break finished, it was time to meet Alan Norrish, and his encyclopaedic knowledge of using drills on people in hot places…
Tea break finished, it was time to meet Alan Norrish, and his encyclopaedic knowledge of using drills on people in hot places…
Some Ugandan studies: 3% of all surgical procedures ended up with osteomyelitis, and 18% of paediatric hospital days was related to joint and bone infection.
In the developing world resources are short, so the focus goes on injuries with blood and bones all over the place, rather than long standing musculoskeletal problems that cause a lot of morbidity.
Often there is not enough time or money to operate, but sometimes Alan has found this website rather helpful for giving patients helpful exercises.
Childhood limb specific disorders
Failure of formation
Hemimelia (picture above right) is missing bones or parts of bones:
- Missing fibula
- Missing tibia (autosomnal dominant)
- Missing radius (causes clubbed hand)
- Missing fingers (claw hand)
Failure of separation
- Most common is syndactyly of the fingers and toes.
- Can be simple with bones separate, or complex with bones combined.
Duplication
- Normally extra fingers and toes.
Amniotic constriction bands
- Need removing before the child grows, as get tighter
Undergrowth of bones
- Shortened femur.
Systemic Congenital Conditions
- Osteogenesis imperfecta
- Fibrodysplasia ossificans progressivica.
- Cerebral palsy
Common problems
Some people spend all their money trying to find a resolution to a long term problem, and sometimes the best you can do is tell them there is no cure, and then they can spend the money on useful things for their life.
Club feet:
- Common in developing world – 1:1000 births.
- Use serial casting in under 3 years
- 3 years to 8 year, needs soft tissue surgery
- 8 years olds onwards need bone surgery.
Osteomyelitis:
- Acute, treatable with antibiotics
- Chronic, will need bone debridement, very difficult to cure.
TB of bones and joints:
- Often present without pulmonary TB.
- Triple therapy is treatment.
Burns & bites:
- Elevate limb and splint joints in functional position.
- The skin can cause a contracture of scar tissue that needs cutting, or serial casting to prevent it limited movement.
Neck injuries:
- Go and hold the neck. It will increase awareness of the neck to other staff.
- Rigid collar.
- Log rolls for moving patient.
- If facet joint dislocation, you can perform head traction!
Burns
 It turns out that I am not very good a paying attention to lectures for 8 days in a row. Eyes practically closed, I grab a coffee with ten sugars in time for the final talk of the morning with Sarah Tucker…
It turns out that I am not very good a paying attention to lectures for 8 days in a row. Eyes practically closed, I grab a coffee with ten sugars in time for the final talk of the morning with Sarah Tucker…
Our three key aims with treating burns in a resource poor setting are survival, prevention of disability and effective use of resources.
We did an audit in Nepal that showed that in six years, no one had survived 40% burns on our burn unit.
Painful as it is to say, this means that it was unlikely to be worth the heavy investment in resources treating people with this level of fatal wound. Burns patients die from injection – sadly we had to make the decision to treat anyone with more than 60% palliatively.
Severity of Burns
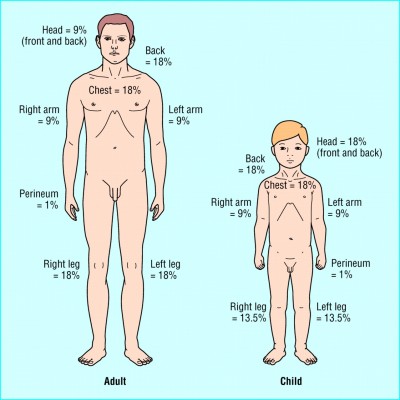
To assess percentage coverage, we use the rule of 9s – click the image on the right for more information.
The best way of finding out depth of a burn is to see how quickly it heals. Anything that heals in less than 2 weeks is superficial, longer is deep.
Treating Burns
You need to perform escarotomies if any circumferential full thickness burns to the limbs, chest or neck, to prevent contractures.
The burn needs to be scrubbed clean, especially if any foreign bodies or chemicals. The burn will need to be scrubbed every few days, this removes dead skin, leaving healthy tissue.
The Ideal Burns Dressing
My pet hate is people arriving from the West with boxes of dressings, that everyone leaps on, gets very excited about, and then runs out. Much better to teach everyone to make local solutions that work well.
- Clean
- Available and sustainable
- Cheap
- Non adherent
- Reduced need for analgesia
- Reduced need for changing
- Antiseptic
We started to use banana leaves for burns dressings. They can be autoclaved, boiled and sterilised. They are non adherent. They work better than silicone dressings.
I showed the banana leave dressings to our nurses, then went away for two weeks. When I came back, they had visited all the trees in the area, autoclaved leaves and filled the fridge with them of their own volition – that’s how noticeable a difference they made to the nurses.

Preventing contractures.
If burns are across joints, and the joint is held out straight, inflammation, then scar tissue will cause contractures, which will cause functional problems in future.
There are some finer points, but generally the Edinburgh position (on the right) will prevent the hand losing functionality.
If there are burns on the inside of the hand, you will need to release the splint at night, or splint it straight at night to prevent this.
Practical Skills Workshop
The afternoon was an exciting blend of Plaster of Paris, Disolocations and traction, Skin grafting and Physio sessions. Afraid there’s not much I can say about them – you had to be there! Since you weren’t, you did miss me accidentally removing the skin on my knuckle whilst practicing taking a skin draft on an orange.



Really starting to flag, on Day Eight of this course. Read @bigonroad’s notes for today: trauma & ortho http://t.co/ESfETAJ9 #cmfdevhealth